DENIAL MANAGEMENT IN HEALTHCARE
Denial management is an epidemic to the financial health of most practices, and they need to be treated well for your practice’s financial success. An estimated 10% of a physician’s revenue is lost due to the lack of denial management.
Billers in our firm are experts in denial management analysis. Our Medical Billers and Coders help in preventing denials and revenue losses in the first place, and also help if you have denials from the past, and get them paid easily.
The process of Denial Management Services has only one key – analysis. Once the root cause of denial is figured, correcting it and getting paid for it is not a task. The skill of a specialist is required to get the perfect analysis of a denial.
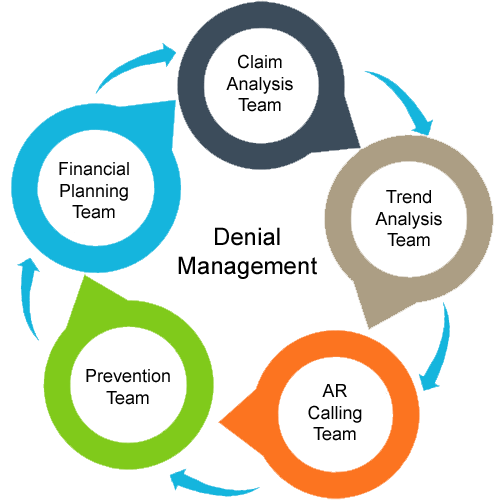
We adopt the following strategies of denial management to improve the medical billing process:
Patient’s Eligibility
Our dedicated staff is well-trained to collect information about each patient’s health insurance eligibility, coverage, and benefits. Our physician practice management system has the modern capability to get and verify eligibility information and benefits even before the patients get admitted.
We have designed a unique process that ensures prior authorization for every needful service. Our experts deeply investigate prior authorization needs for all in-office services that are generally ordered during the patient’s visit and it allows your office staff to know when to obtain specific authorization before rendering a procedure.
Minimize coding errors in denial management services
The conversion of different medical billing services into ICD-10 coding symbols will likely lead to more denials due to an increase in coding errors. At Genesis Diagnostics, we take various proactive steps to reduce coding errors.
We identify and investigate your practice to seek expert advice and add appropriate codes to your practice. Finally, our coding experts thoroughly review and verify codes for any error before submitting each claim.
Analyzing Medical Needs
If a wrong diagnosis code is assigned, then most likely it won’t support the requirements for the provided services and there are more chances that it will be denied by the insurance company.
Therefore, we make use of specialized software for denial management services that not only correct charges to determine insurance coverage but collect policies regarding different medical necessities from all your insurers as well.
Our billers are specially trained to deliver denial management services and recover the collectibles from:
- Worker’s compensation
- Medicare
- Medicaid
- All other major payers like BCBS, Aetna, Cigna, UHC, etc
- Attorneys
Denial claims are eligible for payment of “Appeals” – Appeals are requests and explanations of the claim sent earlier and conditions on which the claim now is again eligible for payment.
Some appeals are time-sensitive. Our Medical Billers review your most commonly denied claims, prioritizing both for volume and dollar value, and file them in a timely manner.
Considering the cost of appealing claims (both in terms of time and money) also helps our medical billers decide whether they must appeal the claim at all. So they will not appeal every claim but know the fact that many practices lose great sums of income every year because they don’t appeal denied claims.
Professional Memberships and Certifications
Trusted and Reliable Denial Management Services:
At Genesis Diagnostics, we speed up the repair and re-submission processes of denied claims. Our intelligent workflow engine provides client-specific and efficient logic for Denial Management Services that includes re-submission of claims to the right departments and also maintaining a detailed history of actions on all claims.
We have over 13 years of experience to serve our clients across the globe with the best denial management services at reasonable prices. We aim to bring down and minimize your number of denied claims within the minimum possible time.